An updated Cochrane review has evaluated the benefits and harms of routine abdominal drainage after pancreatic surgery, the effects of different types of surgical drains, and the optimal time for drain removal.
Main results: 12 RCTs with 2,550 adult participants were included. The studies were published between 2001 and 2023 and conducted in North America, Europe, and Asia. Half of the patients had surgery for pancreatic cancer, and other indications included biliary cancer, duodenal cancer, ampullary cancer, and chronic pancreatitis. Outcomes were synthesised in meta-analyses, and the certainty of the evidence was very low to low for most outcomes.
Pancreaticoduodenectomy
- Drain vs no drain (2 RCTs, 532 participants) and active drain vs passive drain (3 RCTs, 441 participants): Using a drain or not, regardless of the type of drain, may have little to no effect on the risk of mortality, intra-abdominal infection, and wound infection, but the evidence is very uncertain.
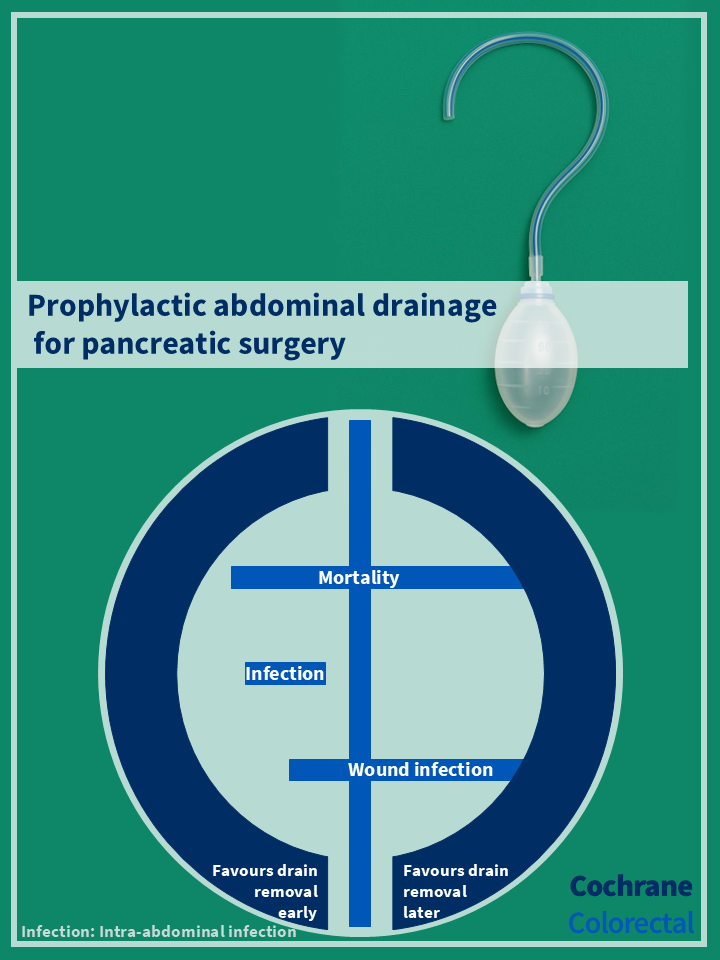
- Early vs late drain removal (3 RCTs, 557 participants with low risk of pancreatic fistula): If using a drain postoperatively, early drain removal probably reduces the risk of intra-abdominal infections compared with late drain removal. The anticipated risk within the first 30 days after the operation was 58 infections per 1,000 participants having early drain removal (95% CI 34 to 102) versus 129 per 1,000 having late drain removal. The evidence suggests that early drain removal results in little to no difference in the risk of mortality and wound infection.
Distal pancreatectomy
- Drain vs no drain (2 RCTs, 626 participants): Using a drain may have little to no effect on the risk of mortality, intra-abdominal infection, and wound infection, but the evidence is very uncertain.
Authors’ conclusion: The evidence is very uncertain about the effect of drain use compared with no drain use on 90‐day mortality, intra-abdominal infection rate, and wound infection rate in people undergoing either pancreaticoduodenectomy or distal pancreatectomy. The evidence is also very uncertain whether an active drain is superior, equivalent, or inferior to a passive drain following pancreaticoduodenectomy. Moderate‐certainty evidence suggests that early drain removal is probably superior to late drain removal in terms of intra-abdominal infection rate following pancreaticoduodenectomy for people with low risk of postoperative pancreatic fistula.
Access the publication here: https://doi.org/10.1002/14651858.CD010583.pub6