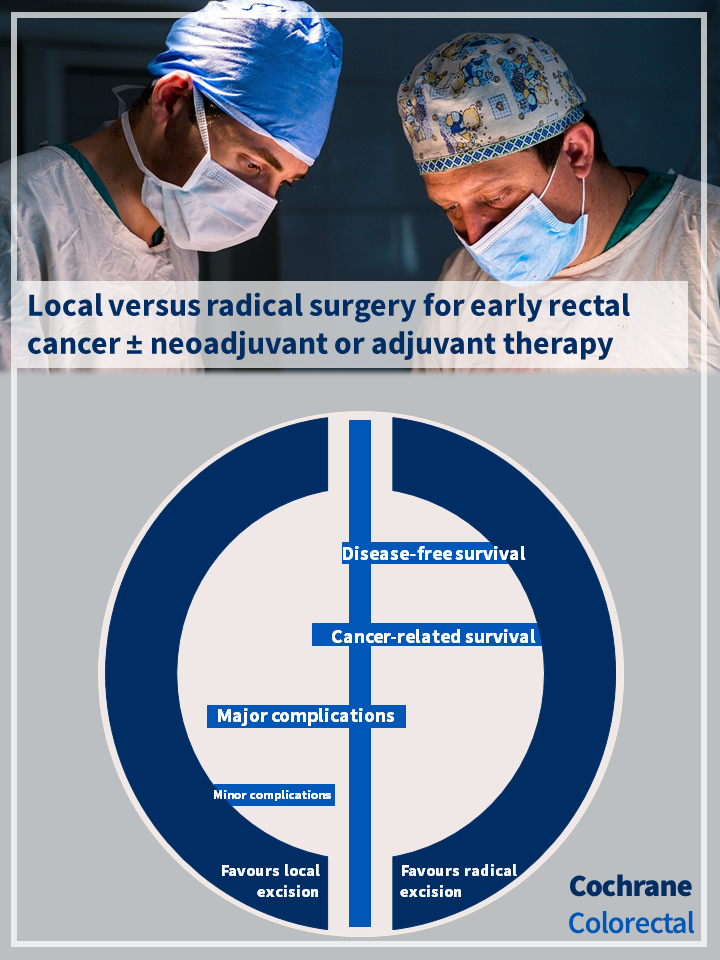
We want to share this Cochrane review: Local versus radical surgery for early rectal cancer with or without neoadjuvant or adjuvant therapy.
Objectives: The objective was to assess the oncologic, operative, and functional outcomes of modern endoscopic local excision compared to radical resection surgery in adults with stage I rectal cancer.
Main results: 4 randomized trials with 266 participants were included.
In this publication, the authors conducted a comprehensive Cochrane systematic review with meta-analyses to assess the effects local versus radical surgery for early rectal cancer with or without neoadjuvant or adjuvant therapy.
The objective was to assess the oncologic, operative, and functional outcomes of modern endoscopic local excision compared to radical resection surgery in adults with stage I rectal cancer.
The rigorous analysis of 4 RCTs involving 266 participants revealed that
- Radical surgery may result in an improvement in disease‐free survival compared to local excision (3 trials, 212 participants; HR 1.96, 95% confidence interval (CI) 0.91 to 4.24). This would translate into a three‐year disease‐recurrence risk of 27% (95% CI 14 to 50%) versus 15% after local excision and RR, respectively.
- At three years, the local excision group had superiority in overall stool frequency, embarrassment about bowel function, and diarrhea.
- Local excision may have little to no effect on cancer‐related survival compared to radical resection (3 trials, 207 participants; HR 1.42, 95% CI 0.60 to 3.33; very low‐certainty evidence).
- The evidence is uncertain about the effect of local excision compared with radical resection on quality of life.
The authors concluded that based on low‐certainty evidence, local excision may decrease disease‐free survival in early rectal cancer. Very low‐certainty evidence suggests that local excision may have little to no effect on cancer‐related survival compared to radical resection for the treatment of stage I rectal cancer. Based on low‐certainty evidence, it is unclear if local excision may have a lower major complication rate, but probably causes a large reduction in minor complication rate.
Access publication here: https://doi.org/10.1002/14651858.CD002198.pub3